Leukocytes are an important part of the immune system that help fight off infection and disease in the body. Usually, only a small number of leukocytes are present in the urine. However, an increased level of leukocytes in the urine can indicate inflammation or infection of the urinary tract, kidneys, or other structures.
Understanding the implications of leukocytes in urine can help guide proper treatment to resolve the underlying condition. This comprehensive overview covers the details of how leukocytes end up in urine, the associated symptoms, and when to see a doctor.
What Are Leukocytes and What Do They Do?
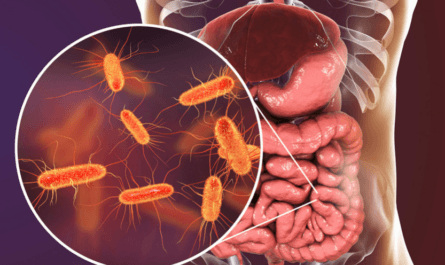
Leukocytes, often called white blood cells (WBCs), are one of the main types of immune cells involved in the body’s response to invasion by foreign organisms or pathogens. The primary role of leukocytes is to defend the body from infection and fight disease.
There are several different types of leukocytes, including:
- Neutrophils – The most common type of white blood cell that engulfs and destroys bacteria and fungi
- Lymphocytes – Include both T cells and B cells involved in the immune response
- Monocytes – Large WBCs that can ingest microbes and become macrophages
- Eosinophils – Help fight parasites and control allergic reactions
- Basophils – Secrete histamine and other chemicals during inflammatory reactions
Normally, leukocytes circulate in the bloodstream and lymphatic system. However, with an infection or inflammatory response, they can move into tissues and organs where pathogens, damaged cells, or other irritants are located. Higher than normal levels of leukocytes may enter the kidneys or urinary tract when fighting an infection in those areas.
What Do Leukocytes in Urine Mean?
The presence of leukocytes in urine, known as leukocyturia, usually indicates some type of inflammation, irritation, or infection occurring in the kidneys, bladder, ureters, urethra, or other areas of the urinary tract.
Some key points about what leukocytes in urine typically signify:
- An elevated level of leukocytes is abnormal and requires further evaluation to determine the cause.
- It often means there is an inflammatory response to an infection somewhere in the urinary system. Common infections that cause leukocytes in urine include urinary tract infections (UTIs), kidney infections, prostatitis, and some sexually transmitted diseases.
- Non-infectious inflammatory conditions like interstitial cystitis and autoimmune disorders can also lead to increased leukocytes in the absence of infection.
- Particularly high leukocyte counts usually correlate with more active or severe inflammation and infection.
- The more leukocytes present, the more likely a bacterial infection is the underlying cause rather than just irritation or injury alone.
- The presence of nitrites and bacteria in urine along with leukocytes further points to a UTI or kidney infection.
- For women, leukocytes in urine most often indicate a UTI, while in men they may signal an inflamed prostate or STD like chlamydia.
- Symptoms accompanying leukocyturia can help identify the location of inflammation such as the bladder or kidneys.
- Persistent leukocytes without infection may be a sign of kidney disease, damage, or cancer needing evaluation.
In general, leukocytes in urine are a key indicator that further diagnostic tests and prompt medical care are required to determine the cause and guide appropriate treatment.

When Should You See a Doctor About Leukocytes in Urine?
It is advisable to see a doctor for evaluation if you have symptoms along with leukocytes in your urine. Even without symptoms, recurring or persistent leukocyturia on multiple urine tests warrants medical assessment to check for potential issues.
You should seek prompt medical care if symptoms like fever over 101°F, vomiting, chills, or shaking develop, as these can indicate a spreading kidney infection. Likewise, back pain accompanied by leukocytes can signal kidney inflammation.
Pregnant women should be evaluated for any leukocytes detected in urine, as they may represent a urinary tract infection that could lead to pregnancy complications if left untreated.
Seeking care is also important for at-risk groups like those over 65, diabetics, or immunocompromised patients in which even minor infections can become serious. Schedule an appointment with your doctor if unexplained leukocytes are found.
Conclusion
In summary, the presence of increased leukocytes in urine typically signifies inflammation or infection of part of the urinary tract. It should not be ignored, as it usually indicates some type of underlying medical condition needing further evaluation and appropriate treatment guided by a physician.
While in some cases leukocyturia may resolve on its own, persistent or recurring cases, especially with symptoms will require proper diagnosis and management. Catching the cause early provides the best chance for effective treatment and prevention of potential complications.