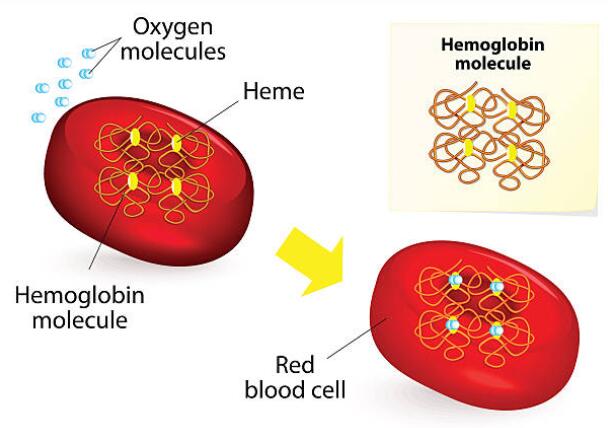
Low hemoglobin count is a common condition affecting millions of people worldwide. Hemoglobin is a protein found in red blood cells that is responsible for carrying oxygen from the lungs to the rest of the body. When the hemoglobin count is low, the body doesn’t get enough oxygen, leading to several health problems.
Symptoms of low hemoglobin count include fatigue, shortness of breath, pale skin, and a rapid heartbeat. While low hemoglobin count can be caused by several factors, including poor nutrition, chronic disease, and certain medications, it is important to seek medical attention if you experience any of these symptoms.
In this article, we will explore the causes, symptoms, and treatment options for low hemoglobin counts and provide tips for improving your hemoglobin levels naturally.
What Does It Mean When Your Hemoglobin Is Low?
When your hemoglobin is low, it means that you have a lower-than-normal number of red blood cells or less hemoglobin than normal in your blood. Hemoglobin is a protein in red blood cells that carries oxygen from your lungs to the rest of your body. When your hemoglobin level is low, your body may not get enough oxygen to function properly.
What is a Normal Hemoglobin Count?
The average Hemoglobin count differs in every individual — Your hemoglobin count changes with age, gender, and certain people.
The normal hemoglobin ranges are:
- Newborns: 17 to 22 gm/dL
- For Men: the average hemoglobin range is between 13.5 to 17.5 grams per deciliter.
- For Women: the average hemoglobin range is between 12.3 and 15.3 gm/dL
What is a Low Hemoglobin Number(Explanation)
- For men, the hemoglobin count falls below 13.5 grams of hemoglobin per deciliter (135 grams per liter) of blood.
- When the count falls below 12 grams per deciliter (120 grams per liter) for women.
In children, low hemoglobin count may vary with sex and age. Women that are pregnant and women having their menstrual period usually have lower hemoglobin counts.
What is a dangerous level of low hemoglobin?
The danger level of low hemoglobin varies depending on the underlying cause and the individual’s overall health. Generally, a hemoglobin level below 7 grams per deciliter (g/dL) is considered severe anemia and may require urgent medical attention.
Severe anemia can cause symptoms such as shortness of breath, fatigue, weakness, rapid or irregular heartbeat, chest pain, and dizziness.
Symptoms of Low Hemoglobin Count
Low hemoglobin count can cause a variety of symptoms. Here are some common symptoms:
- Fatigue and weakness: Anemia can make you feel tired and weak, even after enough rest.
- Shortness of breath: If your body is not getting enough oxygen due to low hemoglobin, you may experience shortness of breath or difficulty breathing.
- Pale skin: Low hemoglobin can cause your skin to become pale or yellowish.
- Dizziness or lightheadedness: Anemia can cause a drop in blood pressure, which can lead to feelings of dizziness or lightheadedness.
- Headaches: Low hemoglobin can cause headaches or migraines.
- Cold hands and feet: If your body is not getting enough oxygen, your extremities may feel cold to the touch.
- Chest pain: In severe cases of anemia, you may experience chest pain or angina.
10 Common Causes of Low Hemoglobin Count
1. Iron Deficiency
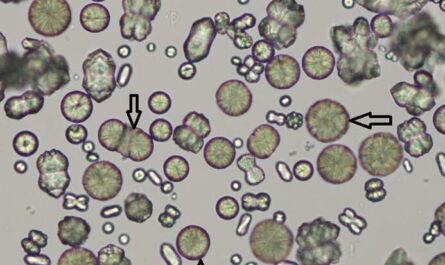
One of the primary causes of low hemoglobin count is iron deficiency. Iron is essential for producing hemoglobin, and when there is a lack of iron in the body, the production of red blood cells is compromised.
This can lead to a decrease in hemoglobin levels. Iron deficiency can be caused by poor dietary intake, malabsorption issues, or blood loss due to menstruation or other reasons.
2. Vitamin B12 Deficiency
Vitamin B12 is another crucial nutrient for maintaining healthy hemoglobin levels. It is involved in the production of red blood cells and helps in the proper functioning of the nervous system.
A deficiency in vitamin B12 can lead to a decrease in red blood cell production, resulting in low hemoglobin levels. Vegetarians and vegans are at a higher risk of developing vitamin B12 deficiency as it is primarily found in animal-based foods.
3. Chronic Kidney Disease
Chronic kidney disease can contribute to low hemoglobin count due to the reduced production of erythropoietin hormone.
Erythropoietin stimulates the production of red blood cells in the bone marrow. In kidney disease, the kidneys cannot produce an adequate amount of this hormone, leading to decreased hemoglobin levels.
4. Chronic Inflammation
Chronic inflammation can disrupt the normal production of red blood cells, leading to low hemoglobin count. Conditions such as rheumatoid arthritis, lupus, and inflammatory bowel disease can cause persistent inflammation, impacting the bone marrow’s ability to produce healthy red blood cells.
5. Blood Loss
Significant blood loss, whether from an injury, surgery, or gastrointestinal bleeding, can result in a low hemoglobin count. When the body loses blood, it also loses red blood cells and hemoglobin. It takes time for the body to replace the lost blood cells, which can lead to a temporary decrease in hemoglobin levels.
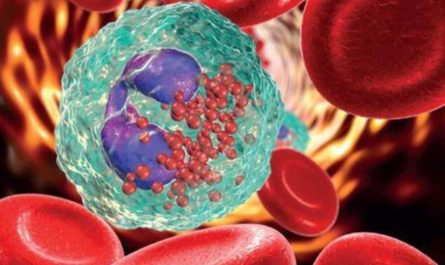
6. Hemolytic Anemia
Hemolytic anemia is a condition characterized by the destruction of red blood cells at a faster rate than the body can replace them. This can lead to a decrease in hemoglobin levels. Hemolytic anemia can be inherited or acquired from factors such as autoimmune disorders, infections, or certain medications.
7. Bone Marrow Disorders
Disorders affecting the bone marrow, such as aplastic anemia and myelodysplastic syndromes, can disrupt the production of red blood cells and lead to low hemoglobin count. In these conditions, the bone marrow fails to produce adequate healthy red blood cells, resulting in decreased hemoglobin levels.
8. Chronic Diseases
Certain chronic diseases, including cancer, HIV/AIDS, and liver disease, can contribute to low hemoglobin counts. These diseases can affect the body’s ability to produce red blood cells or lead to increased destruction of red blood cells, ultimately leading to low hemoglobin levels.
9. Nutritional Deficiencies
Other nutritional deficiencies besides iron and vitamin B12 can also impact hemoglobin levels. Inadequate intake of folate, vitamin C, and other essential nutrients can impair red blood cell production and lead to low hemoglobin count. Maintaining a well-balanced diet rich in fruits, vegetables, and whole grains is crucial for optimal hemoglobin levels.
10. Genetic Factors
In some cases, low hemoglobin count can be attributed to genetic factors. Certain inherited conditions, such as thalassemia and sickle cell disease, can affect the production or structure of hemoglobin, leading to low hemoglobin levels. These conditions require specialized medical management and care.

Best Treatment for Low Hemoglobin Count
How to fix low hemoglobin? This usually depends on the underlying cause. Fortunately, you can treat low mean corpuscular hemoglobin in most cases by making simple lifestyle and dietary changes, especially if you have iron or vitamin-based anemia.
1. Consuming more iron
Iron deficiency anemia is the most common cause of low hemoglobin. Therefore, taking iron-containing foods can effectively improve symptoms.
Iron-rich vegetables mainly include radishes, broccoli, spinach, and kale. You can also eat more liver, eggs, oysters, beef, dried beans, molasses, peanut butter, pork, and whole grains. In addition, dried fruits such as raisins, plums, and dried apricots are good sources of iron.
2. Increasing folate intake
Your body needs a particular type of vitamin B called folate. The folate produces heme, an essential component of hemoglobin that carries oxygen around the body.
When your body lacks adequate folate, your red blood cells won’t reach maturity. This, in turn, affects the production of hemoglobin cells and could lead to folate-deficiency anemia.
You can boost your folate by taking foods including:
- Rice
- Beef
- Spinach
- Peanuts
- Kidney beans
- Black-eyed peas
- Avocadoes
3. Optimizing iron absorption
While taking in foods or supplements rich in iron can boost your hemoglobin count levels, if your body cannot absorb iron properly, it may fall just as fast as it rises.
You can optimize your iron intake by consuming foods that help your body absorb iron. Consuming foods rich in vitamin C helps your body absorb iron and boosts hemoglobin levels.
Leafy green vegetables, citrus fruits, and strawberries are excellent Vitamin C sources. Vitamin A supplements and beta-carotene can help your body absorb and use iron.
Foods that contain vitamin A include:
- Liver
- Fish
- Sweet potatoes
4. Taking iron supplements
Taking iron supplements can help improve the symptoms. Your hemoglobin count will gradually increase over a few weeks as you take the recommended accessories.
However, taking too much iron at once can be counter-effective. Overdosing in iron can cause hemochromatosis and liver disease. In addition, it can also cause constipation, nausea, and vomiting.
5. Treat the underlying condition
If your anemia results from a chronic disease, your doctor will treat the underlying condition. Usually, taking care of the underlying disease will improve your hemoglobin count.
In some rare cases, when the symptoms are severe, your doctor may recommend a blood transfusion or injections of a synthetic hormone (erythropoietin) that might help stimulate red blood cell production and ease fatigue.
- Aplastic anemia
Specific medications and chemotherapy can help to treat aplastic anemia. You may require a blood transfusion to increase the number of red blood cells.
If your bone marrow cannot produce healthy red blood cells, your doctor may have surgery for a bone marrow transplant.
- Hemolytic anemia
Mild hemolytic anemia may not require treatment if the symptoms don’t worsen. Severe hemolytic can be life-threatening if not treated correctly and usually requires ongoing treatment.
To treat chronic hemolytic anemia, the patient may require medications that suppress the immune system, which could attack her red blood cells. You may also need blood transfusions, bone marrow transplants, or surgery.
Common Questions:
1. How is low hemoglobin count diagnosed?
Low hemoglobin count can be diagnosed through a simple blood test called a complete blood count (CBC). This test measures the number of red blood cells and the amount of hemoglobin in the blood.
2. Can low hemoglobin count be prevented?
In some cases, low hemoglobin count can be prevented by maintaining a healthy diet rich in iron and other essential nutrients, avoiding excessive alcohol consumption, and treating underlying medical conditions that can cause anemia.
It’s important to speak with a doctor about any concerns related to low hemoglobin count and to follow recommended preventative measures.
3. Is low hemoglobin count dangerous?
In some cases, low hemoglobin count can be dangerous if left untreated or if the underlying cause is serious. Anemia can lead to complications such as fatigue, shortness of breath, heart problems, and other health issues. It’s important to address low hemoglobin count promptly to prevent potential complications.
4. How long does it take for hemoglobin levels to improve?
The time it takes for hemoglobin levels to improve depends on the underlying cause and the treatment provided. With proper treatment and management, it is possible to see an improvement in hemoglobin levels within a few weeks to a few months.