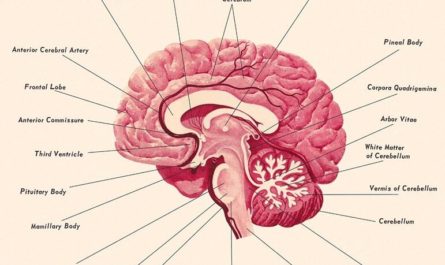
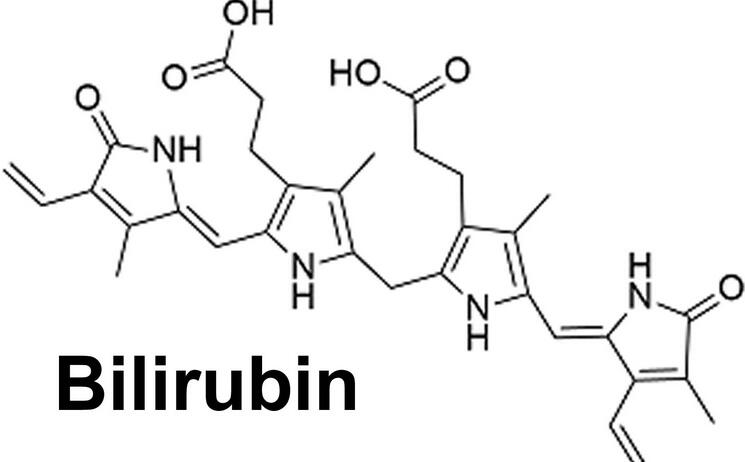
Bilirubin is a byproduct of the breakdown of heme. It is found in hemoglobin, the molecule responsible for carrying oxygen in red blood cells. When red blood cells reach the end of their lifespan, they are broken down in the liver, spleen, and bone marrow. Bilirubin is released during this process and is transported to the liver, where it undergoes further processing and is eventually excreted in bile.
The normal range of bilirubin in the blood is typically between 0.2 and 1.2 milligrams per deciliter (mg/dL). When bilirubin levels exceed this range, it can lead to a condition known as hyperbilirubinemia. This excess bilirubin can then be detected in the urine, indicating a potential problem.
Bilirubin in Urine: What Does It Mean?
The presence of bilirubin in urine can indicate a potential issue with the liver or bile ducts. Bilirubin is a yellow pigment that is produced when red blood cells break down. It is normally processed by the liver and excreted in the bile, which then enters the digestive tract. When bilirubin is present in urine, it may suggest decreased liver function or obstruction of the bile ducts.
Does bilirubin in the urine always indicate liver problems?
No, bilirubin in the urine does not always indicate liver problems. A large number of people have small amounts of bilirubin in their urine without any significant health problems. The presence of bilirubin in the urine could mean that you have a liver problem and require further testing. However, it is not a definitive test for liver disease.
Bilirubin in urine during pregnancy
Higher bilirubin levels during pregnancy usually indicate that a pregnant woman’s red blood cells are not working correctly. Gallbladder disease and Hepatitis may cause this condition. You should consult a doctor as soon as possible for a comprehensive examination.
High Levels of Bilirubin
High levels of bilirubin in the blood, also known as hyperbilirubinemia, can be indicative of different underlying conditions. The reference range for total bilirubin levels may vary slightly between laboratories, but generally, levels greater than 1.2 mg/dL (milligrams per deciliter) are considered elevated.
Hyperbilirubinemia can be further categorized into unconjugated (indirect) bilirubin and conjugated (direct) bilirubin:
- Unconjugated bilirubin: Levels above 1 mg/dL are typically considered high. This may be seen in conditions such as hemolytic anemia, Gilbert’s syndrome, or certain liver diseases.
- Conjugated bilirubin: Levels above 0.3 mg/dL are often considered elevated. Conjugated bilirubin is bound to a substance called glucuronic acid in the liver and is excreted in bile. Elevated levels of conjugated bilirubin may indicate liver diseases or bile duct obstruction.
It’s important to note that the interpretation of bilirubin levels should be done in conjunction with a healthcare professional, as additional factors, such as clinical symptoms and other liver function tests, need to be considered for an accurate diagnosis.
Low Levels of Bilirubin
Low levels of bilirubin in the blood, also known as hyperbilirubinemia, are less common and may not be as extensively studied as high levels. The reference range for low levels may also vary between laboratories.
Generally, bilirubin levels below 0.3-0.4 mg/dL are considered low. Low levels of bilirubin may occur in conditions that affect bilirubin metabolism, such as certain medications or genetic disorders like Dubin-Johnson syndrome.
What are the symptoms of Bilirubin in Urine?
The presence of bilirubin in urine itself does not cause specific symptoms. However, the underlying conditions or factors causing bilirubinuria can lead to various symptoms. Here are some potential symptoms associated with bilirubin in urine:
- Jaundice: Jaundice is a yellowing of the skin and eyes that can occur when there is a buildup of bilirubin in the body. It is a common symptom of liver diseases, gallstones, or other conditions that can cause bilirubinuria.
- Dark urine: Bilirubin can give urine a darker color, ranging from amber to brown. This change in urine color is often noticeable when there is an increased level of bilirubin in the urine.
- Pale stools: When bilirubin is not properly excreted into the digestive tract due to liver or bile duct issues, stools may become pale or clay-colored. This occurs because bilirubin is responsible for the normal brown color of stools.
- Abdominal pain: Some conditions that cause bilirubinuria, such as gallstones or pancreatic disorders, can lead to abdominal pain or discomfort. The pain may be localized in the upper right abdomen or radiate to the back.
- Fatigue and weakness: Liver diseases or other conditions affecting bilirubin metabolism can result in fatigue, weakness, and a general feeling of being unwell. This can be due to compromised liver function and the buildup of toxins in the body.
- Nausea and vomiting: In cases where bilirubinuria is associated with liver diseases or gallstones, individuals may experience nausea and vomiting. These symptoms can be related to the underlying condition or the bile flow obstruction.
- Itching: Excess bilirubin in the bloodstream can cause generalized itching, also known as pruritus. Itching is often more pronounced in areas with thinner skin, such as the palms and soles.
It is important to note that not everyone with bilirubin in urine will experience all of these symptoms. The presence of bilirubin in urine should always be evaluated by a healthcare professional to determine the underlying cause and appropriate treatment.

Bilirubin in Urine: 10 Causes with Treatment
Here are 10 causes of bilirubinuria and their respective treatments.
1. Hepatitis
Hepatitis is one of the main causes of bilirubin in the urine. Inflammation of the liver, caused by viral infections or other factors, can impair the liver’s ability to process bilirubin effectively, leading to a buildup of conjugated bilirubin in the blood and urine.
Treatment: The treatment for hepatitis depends on the specific type of viral infection (e.g., hepatitis A, B, or C) and the severity of the condition. Antiviral medications, supportive care, and lifestyle modifications (e.g., avoiding alcohol, and maintaining a healthy diet) are common approaches to managing hepatitis and reducing bilirubin levels.
2. Cirrhosis
Cirrhosis is a condition characterized by scarring of the liver tissue, which can result from various factors such as alcohol abuse, viral hepatitis, or non-alcoholic fatty liver disease. As the liver’s function deteriorates, it may struggle to process bilirubin, causing bilirubinuria.
Treatment: Treatment for cirrhosis focuses on managing the underlying cause, preventing further liver damage, and addressing complications such as portal hypertension and liver failure. This may involve alcohol cessation, antiviral therapy, nutritional support, and in severe cases, liver transplantation.
3. Gallstones
Gallstones can obstruct the bile ducts, preventing bilirubin from being excreted properly. This can lead to a buildup of bilirubin in the blood and its eventual appearance in the urine.
Treatment: Treatment for gallstones typically involves surgical removal of the gallbladder (cholecystectomy) or endoscopic procedures to remove the stones and restore bile flow. In some cases, medications may be used to dissolve small gallstones.
4. Bile Duct Obstruction
Apart from gallstones, other factors such as tumors, cysts, or inflammation can obstruct the bile ducts, leading to a backup of bilirubin in the system and its presence in the urine.
Treatment: Treatment for bile duct obstruction depends on the underlying cause. Surgical removal of tumors or cysts, endoscopic procedures to place stents or remove obstructions, and medications to manage inflammation may be necessary.
5. Certain Medications
Some medications, such as antibiotics, can cause liver damage or interfere with bilirubin metabolism, resulting in bilirubinuria.
Treatment: If a medication is identified as the cause of bilirubinuria, adjusting the dosage or switching to an alternative medication may be necessary. Close monitoring of liver function and bilirubin levels is important when using potentially hepatotoxic drugs.
6. Genetic Disorders
Rare genetic disorders that affect the liver’s ability to process bilirubin, such as Gilbert’s syndrome or Dubin-Johnson syndrome, can lead to elevated bilirubin levels in the blood and urine.
Treatment: Treatment for genetic disorders causing bilirubinuria is typically supportive, as these conditions are often benign and do not cause significant liver damage. Lifestyle modifications, such as avoiding fasting and managing stress, may help reduce bilirubin levels.
7. Pancreatic Cancer
Pancreatic cancer can cause bilirubinuria by obstructing the bile ducts, leading to a buildup of bilirubin in the blood and urine.
Treatment: Treatment for pancreatic cancer may involve surgical removal of the tumor, chemotherapy, radiation therapy, or a combination of these approaches. Palliative care measures may be necessary to manage symptoms and improve quality of life.
8. Primary Sclerosing Cholangitis (PSC)
PSC is a chronic inflammatory condition that leads to scarring and narrowing of the bile ducts, causing a buildup of bilirubin in the blood and urine.
Treatment: Treatment for PSC focuses on managing symptoms, preventing complications, and slowing disease progression. This may involve medications to manage inflammation, antibiotics to treat infections, and endoscopic procedures to dilate narrowed bile ducts. In advanced cases, liver transplantation may be necessary.
9. Alcoholic Liver Disease
Excessive alcohol consumption can lead to liver damage and impaired bilirubin metabolism, resulting in bilirubinuria.
Treatment: Treatment for alcoholic liver disease involves alcohol cessation, nutritional support, and management of complications such as cirrhosis and liver failure. Counseling and support groups may be beneficial in maintaining long-term sobriety.
10. Hemolytic Anemia
Hemolytic anemia is a condition characterized by the premature destruction of red blood cells. This can lead to increased production of bilirubin and its presence in the urine[4].
Treatment: Treatment for hemolytic anemia depends on the underlying cause. This may involve medications to suppress the immune system, blood transfusions to replace damaged red blood cells, and treatment of any underlying infections or disorders that may be contributing to the condition.
When should you see a doctor?
The first thing you would do is to check your blood levels of bilirubin. The normal range is 0-50 mg/dL. Anything higher than that means you are getting into dangerous territory, and it is time to see your doctor about it.
You can also use a home test kit for this purpose, but if you have any doubts or questions, you should go directly to the nearest hospital or clinic.
If you notice or observe any persistent symptoms of bilirubin in your urine or body, you must see a doctor immediately. If left untreated, bilirubin in urine can lead to jaundice, anemia, and other health complications.