Urinary tract infections (UTIs) are a common health issue, and one of the most prevalent causes is Escherichia coli (E. coli) bacteria. This article will delve into the topic of E. coli in urine culture, exploring its causes, symptoms, and treatment options. By understanding the intricacies of E. coli UTIs and the importance of urine culture in diagnosing them, you can take proactive steps toward prevention and seek appropriate treatment when needed.
Key Takeaways
- E. coli bacteria can cause UTIs and it enters the urinary tract through different ways like bad wiping, sex, or using a catheter.
- Symptoms of an E. coli UTI include pain when peeing, smelly urine that looks cloudy, belly pain, and sometimes fever.
- To find out if you have an E. coli UTI, doctors will test your pee with a urinalysis or urine culture.
- Antibiotics are used to treat E. coli UTIs but drinking lots of water helps too. Preventing these infections means staying clean and not holding in pee for too long.
- Not treating an E. coli UTI can lead to bigger problems like kidney infections. Some people are more at risk than others for getting these infections.
What is E. Coli?
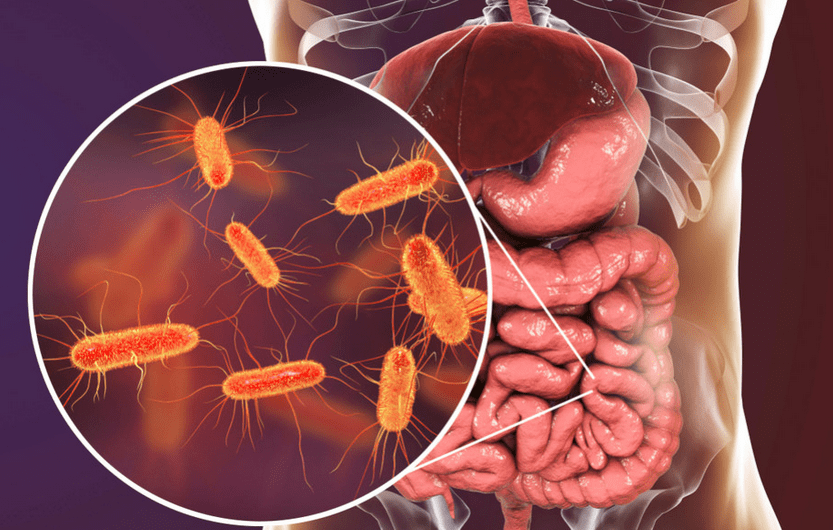
E. coli is short for Escherichia coli, a type of bacteria often found in the guts of people and animals. Most kinds are harmless and are part of the healthy bacterial flora in our bodies.
Some can make you sick, though, causing symptoms like diarrhea or urinary tract infections (UTIs). These germs live in fecal matter. If E. coli spreads from an unclean area to the bladder, it can cause a UTI.
People get these infections when the bacteria enter any part of their urinary system, which includes kidneys, ureters, bladder, and urethra. Good hygiene helps keep E. coli from spreading to these parts of the body where they can cause trouble.
Remembering to wipe correctly after using the bathroom is one way to avoid getting a UTI caused by this bug.
Ways E. Coli enters the urinary tract
E. Coli, commonly found in the gastrointestinal tract, can enter the urinary system through the urethra and spread to the bladder and other parts of the urinary tract. This bacterium gains access primarily through improper wiping after bowel movements, sexual intercourse, or contaminated hygiene products such as toilet paper.
In addition to these modes of entry, E. Coli can also make its way into the urinary tract via catheterization or medical procedures involving the urinary system. Once inside, it multiplies and causes infections that lead to various symptoms associated with UTIs.
Diagnosing E. coli with Urine Culture
A urine culture is a diagnostic test used to identify the presence of bacteria, including E. coli, in the urinary tract. The process involves obtaining a urine sample, culturing it in a laboratory setting, and observing bacterial growth. This test helps determine the specific bacteria causing the infection and guides appropriate treatment decisions.
To perform a urine culture, a clean-catch midstream urine sample is typically collected. This involves thoroughly cleaning the genital area and collecting a midstream portion of urine in a sterile container. The sample is then sent to a laboratory for analysis.
In the laboratory, the urine sample is streaked onto agar plates that support bacterial growth. These plates are incubated at a specific temperature to promote the growth of any bacteria present in the sample. After a designated period, typically 24 to 48 hours, the plates are examined for bacterial colonies.
Interpreting Urine Culture Results
Interpreting urine culture results involves assessing the colony-forming units (CFUs) per milliliter of urine. A higher CFU count indicates a greater bacterial load and suggests an active infection. A positive urine culture for E. coli confirms the presence of this bacteria in the urinary tract, supporting the diagnosis of an E. coli UTI.
It is important to note that the interpretation of urine culture results also takes into account the patient’s symptoms. A culture with a lower CFU count may still be considered positive if the patient exhibits classic UTI symptoms. On the other hand, a culture with a higher CFU count may be considered insignificant if the patient is asymptomatic.
Causes and Risk Factors for E. coli in Urine
E. coli gains access to the urinary system through various pathways. The most common route is through the urethra, which serves as a conduit for urine excretion. Factors that can contribute to the entry of E. coli into the urinary tract include:
- Poor hygiene practices: Inadequate wiping technique after using the toilet, especially in females, can introduce E. coli from the anal area into the urethra.
- Sexual activity: Sexual intercourse can introduce bacteria into the urethra, increasing the risk of UTIs.
- Catheter use: Indwelling urinary catheters, commonly used in healthcare settings, provide a direct pathway for bacteria to enter the bladder.
Understanding these routes of entry can aid in implementing preventive measures.
Who Is at Greater Risk?
Certain populations have a higher risk of developing E. coli UTIs. These include:
- Women: Women have a shorter urethra than men, which makes it easier for bacteria to reach the bladder. Additionally, hormonal changes during pregnancy and menopause can increase the risk of UTIs.
- Elderly individuals: Age-related changes in the urinary tract, weakened immune systems, and underlying medical conditions can make the elderly more susceptible to E. coli UTIs.
- Individuals with compromised immune systems: Conditions such as diabetes, HIV/AIDS, and certain autoimmune disorders can weaken the immune system, making individuals more prone to infections.
- Anatomical abnormalities: Structural abnormalities in the urinary tract, such as urinary tract obstructions or vesicoureteral reflux, can increase the risk of UTIs.
Recognizing these risk factors can help target preventive strategies more effectively.
Treatment and Prevention of E. Coli UTIs
Traditional treatment for E. coli UTIs often involves antibiotics such as trimethoprim-sulfamethoxazole, nitrofurantoin, or fosfomycin. These antibiotics help to kill the E. coli bacteria causing the infection and alleviate symptoms like abdominal cramps and painful urination.
It is important to complete the full course of antibiotics as prescribed by a healthcare provider to ensure that the infection is fully eradicated from the urinary tract. In addition to antibiotic treatment, increasing fluid intake can also help flush out the bacteria from the urinary system.
Remember not all treatments are suitable for everyone since some E. coli strains have developed resistance to certain antibiotics due to overuse and misuse of these medications in both human and animal healthcare settings.
Ways to prevent E. Coli UTIs
Preventing E. Coli UTIs involves practicing good hygiene, wiping from front to back after using the bathroom, and staying well-hydrated. Emptying the bladder frequently and completely can also help flush out any bacteria that may be present.
Additionally, avoiding holding urine for long periods and urinating before and after sexual activity can reduce the risk of E. Coli entering the urinary tract.
Maintaining good personal hygiene is crucial in preventing E. Coli UTIs. This includes regular handwashing with soap and water, especially before handling food or after using the restroom.
Risk factors for acquiring an E. Coli UTI
Certain risk factors can make individuals more susceptible to acquiring an E. Coli UTI. These include being female, having a history of UTIs, using certain types of birth control, menopause, urinary tract abnormalities, kidney stones, a suppressed immune system due to conditions like diabetes or HIV/AIDS, and recent urinary procedures or catheter use.
Moreover, sexual activity and the use of spermicidal agents can also increase the risk of developing an E. Coli UTI.
These risk factors facilitate the entry of Escherichia coli into the urinary tract and can lead to infections if not managed effectively. Understanding these risk factors is crucial in taking preventive measures and seeking timely medical intervention when needed- especially for individuals with these predisposing conditions.
Potential complications
E. coli UTIs can lead to serious complications if left untreated, including kidney infection and bloodstream infection. These complications may cause severe pain, fever, and even life-threatening conditions.
It’s important to seek prompt medical attention if you experience symptoms of a UTI to prevent these potential complications.
In some cases, E. coli bacteria can develop resistance to antibiotics, making treatment more challenging and prolonging the duration of the infection. This can lead to recurrent or chronic UTIs, requiring alternative treatment approaches and close monitoring by healthcare professionals for effective management.
Outbreaks and recalls related to E. Coli contamination
When E. Coli contamination outbreaks occur, it can lead to widespread concerns about food safety and public health. The contamination of food products or water sources with E. Coli can result in recalls by regulatory authorities and manufacturers to prevent the spread of infection and illness caused by this bacteria, highlighting the importance of stringent hygiene and safety measures in food production and distribution.
Innovative treatments and prevention methods for E. Coli UTIs continue to be studied and developed, aiming to improve patient outcomes while also addressing antibiotic resistance concerns associated with conventional treatment options.
Recent outbreaks related to E. Coli contamination serve as a reminder of the ongoing need for effective preventive strategies and prompt responses to minimize the impact on affected individuals and communities at risk.
Innovative treatments and prevention methods
New treatments for E. coli UTIs are being researched, including vaccines that target specific E. coli strains to prevent infections. Some promising prevention methods involve the use of probiotics and cranberry products to inhibit the adherence of E.
coli to the urinary tract, reducing the risk of infection. Additionally, researchers are exploring new antimicrobial compounds and alternative therapies that could offer effective treatment options while minimizing antibiotic resistance.
Innovative approaches such as bacteriophage therapy, which uses viruses to target and destroy harmful bacteria like E. coli, show potential in treating UTIs caused by antibiotic-resistant strains.
FAQ
1. How Long Does It Take for Symptoms to Appear After E. coli Exposure?
The incubation period for E. coli UTIs can vary, but symptoms typically appear within one to three days after exposure. However, in some cases, symptoms may take longer to manifest, so it is important to be vigilant and seek medical attention if any concerning symptoms arise.
2. Can E. coli UTIs Be Prevented Entirely?
While it may not be possible to prevent UTIs entirely, implementing preventive measures can significantly reduce the risk. By practicing good hygiene, staying hydrated, and maintaining a healthy lifestyle, individuals can minimize their susceptibility to E. coli UTIs.
3. What Are the Long-Term Effects of Recurrent UTIs?
Recurrent UTIs, if left untreated or poorly managed, can lead to chronic kidney infections and potentially cause kidney damage. It is important to address recurrent UTIs promptly to prevent long-term complications.
4. How Can I Tell If My UTI Is Caused by E. coli?
A definitive diagnosis of E. coli UTIs requires a urine culture test. This test identifies the specific bacteria causing the infection, including E. coli. If you suspect a UTI, it is crucial to consult a healthcare professional for proper diagnosis and treatment. They will be able to evaluate your symptoms, perform the necessary tests, and provide appropriate treatment options based on the results.
When to See a Doctor?
You should seek prompt medical attention if you have any symptoms of a kidney infection such as:
- Fever over 101°F (38°C)
- Chills and shaking
- Nausea and vomiting
- Severe pain in the back, side, or groin
- Confusion or mental changes
- Fatigue and weakness
Also, see your doctor if UTI symptoms persist or return shortly after antibiotic treatment. Recurring or chronic UTIs require further evaluation and specialized treatment to prevent complications like kidney damage.
Don’t hesitate to contact your healthcare provider if you suspect an E. coli UTI based on painful urinary symptoms. Proper diagnosis and treatment are important, especially for those at higher risk of complications like pregnant women, diabetics, elderly patients, and those with weakened immune systems.






