Pancreatitis is a condition characterized by inflammation of the pancreas. This is a painful and potentially serious digestive disorder. One of the most common symptoms associated with pancreatitis is abdominal pain, which can often radiate to the back. This leads many people to wonder, “Does pancreatitis cause back pain?”
The short answer is yes, pancreatitis can indeed cause back pain. When the pancreas becomes inflamed, it can cause pain in the upper abdominal region that frequently radiates to the back. This is typically felt in the middle or left side of the back.
Understanding the connection between pancreatitis and back pain is crucial for proper diagnosis and treatment. In this article, we will delve into the causes, and symptoms of pancreatitis, and explore the link between this condition and back pain.

What is the Pancreas?
The pancreas is a long, flat gland located behind the stomach in the upper abdomen. It plays a crucial role in digestion and blood sugar regulation by producing enzymes that help break down food and hormones like insulin that control blood sugar levels.
There are two main types of pancreatitis: acute and chronic.
Acute pancreatitis is a sudden inflammation of the pancreas that can range from mild to life-threatening. It often requires hospitalization and can be triggered by a variety of factors, including gallstones, heavy alcohol use, and certain medications.
Chronic pancreatitis, on the other hand, is a long-term condition that develops gradually over time. It occurs when the pancreas becomes permanently damaged, often as a result of repeated episodes of acute pancreatitis or long-term alcohol abuse.
Chronic pancreatitis can lead to serious complications, including diabetes, malnutrition, and even pancreatic cancer.
Why Does Pancreatitis Cause Back Pain?
The pancreas is located deep within the abdomen, surrounded by a complex network of organs, muscles, and nerves. When the pancreas becomes inflamed, it can irritate the nerves in the surrounding area, leading to referred pain in the back.
The type of back pain associated with pancreatitis can vary from person to person. Some describe it as a dull, constant ache, while others experience sharp, shooting pains.
The pain may be localized to a specific area of the back, such as the upper or middle back. Or it may radiate to other parts of the body, like the shoulders or chest.
The back pain may worsen after eating, particularly if the meal is high in fat. Because this stimulates the pancreas to produce more digestive enzymes.
Other Symptoms to Watch For
In addition to back pain, pancreatitis can cause a wide range of other symptoms. These may include:
- Severe abdominal pain: This is the most common symptom of pancreatitis and is often described as a burning or stabbing sensation that radiates to the back.
- Nausea and vomiting: Inflammation of the pancreas can cause the body to release toxins that irritate the digestive system, leading to nausea and vomiting.
- Fever and chills: Pancreatitis can cause a systemic inflammatory response that leads to fever and chills.
- Rapid heartbeat: Inflammation and pain can cause the heart to beat faster than normal.
- Swollen or tender abdomen: As the pancreas becomes inflamed, it can cause the abdomen to swell and become tender to the touch.
- Jaundice: In some cases, pancreatitis can cause a buildup of bilirubin in the blood, leading to yellowing of the skin and eyes (jaundice).
- Unexplained weight loss: Chronic pancreatitis can interfere with the body’s ability to digest food and absorb nutrients, leading to unintended weight loss.
If you experience any of these symptoms, especially if they are severe or persistent, it’s important to seek medical attention right away. Pancreatitis can be a serious condition that requires prompt treatment to prevent complications.
Causes and Risk Factors for Developing Pancreatitis
Several factors can increase your risk of developing pancreatitis. Some of the most common include:
1. Gallstones
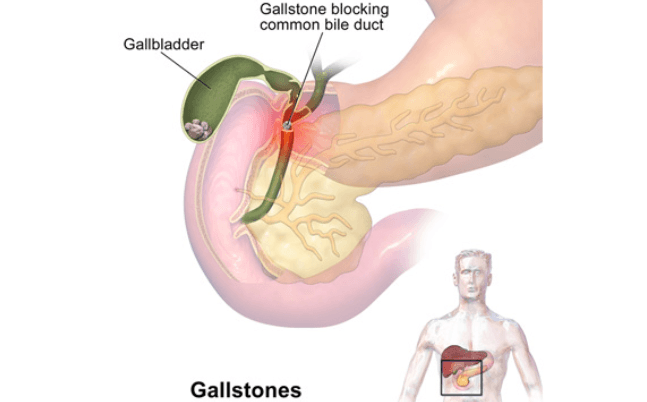
Gallstones are one of the most common causes of acute pancreatitis, accounting for up to 40% of cases. They are small, hard deposits that form in the gallbladder, a small organ that stores bile. When gallstones block the ducts that carry digestive enzymes from the pancreas to the small intestine, it can cause the pancreas to become inflamed.
Symptoms of gallstone pancreatitis may include:
- Sudden, severe pain in the upper abdomen that may radiate to the back
- Nausea and vomiting
- Fever and chills
- Jaundice (yellowing of the skin and eyes)
Treatment for gallstone pancreatitis typically involves hospitalization, pain management, and sometimes surgery to remove the gallbladder and any remaining stones. To reduce your risk of developing gallstones, maintain a healthy weight, eat a balanced diet, and exercise regularly.
2. Alcohol Use
Heavy alcohol use is another leading cause of pancreatitis, particularly chronic pancreatitis. Alcohol is responsible for up to 70% of chronic pancreatitis cases. When you drink alcohol, it can cause the pancreas to produce more digestive enzymes than normal. Over time, this can lead to inflammation and damage to the pancreas.
Symptoms of alcohol-related pancreatitis may include:
- Abdominal pain that may radiate to the back
- Nausea and vomiting
- Weight loss
- Oily or fatty stools
If you have pancreatitis related to alcohol use, it’s important to stop drinking completely to prevent further damage to your pancreas. Your doctor may also recommend pain management, dietary changes, and enzyme supplements to help manage your symptoms.
3. Smoking
Smoking is a significant risk factor for both acute and chronic pancreatitis. Studies have shown that smokers are up to three times more likely to develop pancreatitis than non-smokers. Smoking can damage the pancreas in several ways, including:
- Reducing blood flow to the pancreas
- Increasing the risk of gallstones
- Causing oxidative stress and inflammation
Symptoms of smoking-related pancreatitis are similar to those caused by other factors and may include abdominal pain, nausea, and vomiting.
Quitting smoking is one of the best things you can do to reduce your risk of pancreatitis and other serious health problems.

4. High Triglyceride Levels
Triglycerides are a type of fat found in the blood. When triglyceride levels become too high, it can increase the risk of acute pancreatitis. High triglycerides can be caused by a variety of factors, including:
- Obesity
- Poorly controlled diabetes
- Certain medications (such as birth control pills or steroids)
- Genetic disorders
Symptoms of high triglyceride pancreatitis may include:
- Severe abdominal pain
- Nausea and vomiting
- Fever
- Rapid heartbeat
Treatment for high triglyceride pancreatitis typically involves hospitalization, pain management, and IV fluids. Your doctor may also recommend medications to help lower your triglyceride levels.
5. Autoimmune Disorders
In rare cases, pancreatitis can be caused by an autoimmune disorder, such as lupus or rheumatoid arthritis. In autoimmune pancreatitis, the body’s immune system mistakenly attacks the pancreas, causing inflammation and damage.
Symptoms of autoimmune pancreatitis may include:
- Abdominal pain
- Jaundice
- Weight loss
- Fatigue
Treatment for autoimmune pancreatitis typically involves medications to suppress the immune system, such as steroids or immunomodulators.
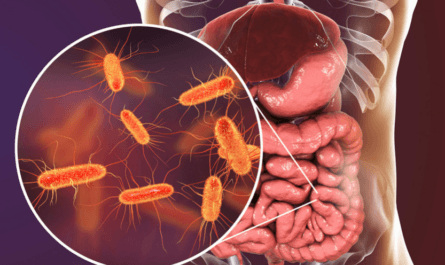
6. Infections
Certain infections, such as mumps or cytomegalovirus, can sometimes cause pancreatitis, particularly in children. When the pancreas becomes infected, it can become inflamed and cause symptoms like abdominal pain, fever, and nausea.
Treatment for infection-related pancreatitis typically involves antibiotics to clear the infection and supportive care to manage symptoms. In severe cases, hospitalization may be necessary.
7. Trauma
Trauma to the abdomen, such as from a car accident or severe fall, can sometimes cause pancreatitis. When the pancreas is injured, it can become inflamed and cause symptoms like abdominal pain and vomiting.
Treatment for trauma-related pancreatitis depends on the severity of the injury and may include hospitalization, pain management, and surgery.

8. Medications
Certain medications, such as diuretics, antibiotics, and immunosuppressants, have been linked to an increased risk of pancreatitis. These medications can sometimes cause the pancreas to become inflamed. This will lead to symptoms like abdominal pain and nausea.
If you develop pancreatitis while taking a medication, your doctor may recommend stopping the medication or switching to an alternative. They may also recommend supportive care to manage your symptoms and prevent complications.
Treatment Options for Pancreatitis
The treatment for pancreatitis depends on the severity of the condition and the underlying cause. In most cases, treatment involves a combination of pain management, dietary changes, and addressing any underlying issues.
1. Acute Pancreatitis Treatment
For acute pancreatitis, treatment may include:
- Hospital stay: Most people with acute pancreatitis need to be hospitalized for close monitoring and supportive care, such as IV fluids and pain medication.
- Fasting: To give the pancreas a chance to rest and heal, you may need to avoid eating or drinking for a few days. You may receive nutrients through an IV during this time.
- Pain management: Your doctor may prescribe pain medication to help manage your symptoms. In some cases, a nerve block or other pain management techniques may be used.
- Treating underlying causes: If your pancreatitis is caused by an underlying issue like gallstones or alcohol use, your doctor will work to address these factors to prevent future attacks.
2. Chronic Pancreatitis Treatment
For chronic pancreatitis, treatment may involve:
- Dietary changes: Eating a low-fat diet and avoiding alcohol can help manage symptoms and prevent further damage to the pancreas. Your doctor may also recommend a diet high in protein and calories to help you maintain a healthy weight.
- Pain management: Chronic pain is a common issue for people with chronic pancreatitis, and your doctor may recommend medications or other therapies to help manage it. This may include over-the-counter pain relievers, prescription pain medications, or alternative therapies like acupuncture or massage.
- Enzyme supplements: If your pancreas is not producing enough digestive enzymes, your doctor may prescribe supplements to help your body break down and absorb nutrients from food. These supplements are taken with meals and snacks to aid in digestion.
- Surgery: In some cases, surgery may be necessary to remove damaged tissue, drain fluid from the pancreas, or widen blocked ducts. Procedures like a pancreatic resection or a Whipple procedure may be recommended for severe cases.
3. Lifestyle Changes for Managing Pancreatitis
In addition to medical treatment, there are several lifestyle changes you can make to help manage pancreatitis and prevent future attacks. These include:
- Avoiding alcohol: If you have pancreatitis, it’s important to avoid alcohol completely, as even small amounts can trigger an attack.
- Quitting smoking: Smoking can increase your risk of pancreatitis and other serious health problems. If you smoke, talk to your doctor about ways to quit.
- Eating a healthy diet: Focus on eating a diet low in fat and high in fruits, vegetables, whole grains, and lean protein. Avoid fried, greasy, or sugary foods that can trigger symptoms.
- Staying hydrated: Drink plenty of water and other clear fluids to help prevent dehydration and keep your digestive system running smoothly.
- Managing stress: Stress can exacerbate pancreatitis symptoms, so it’s important to find healthy ways to manage stress, such as through exercise, meditation, or therapy.
- Getting regular check-ups: If you have chronic pancreatitis, it’s important to see your doctor regularly for check-ups and monitoring. This can help catch any complications early and ensure that your treatment plan is working effectively.
When to Seek Medical Attention?
Pancreatitis can be a serious condition that requires prompt medical attention. If you experience any of the following symptoms, it’s important to seek medical care right away:
- Severe abdominal pain that lasts for more than a few hours or gets worse over time
- Pain that radiates to your back or chest
- Nausea and vomiting that won’t stop
- Fever and chills
- Yellowing of the skin or eyes
- Rapid heartbeat or shortness of breath
- Dizziness or fainting
These symptoms can be a sign of a severe case of pancreatitis or other serious complications, such as infection, kidney failure, or shock. Prompt treatment is essential to prevent long-term damage to the pancreas and other organs.
FAQs
1. Can pancreatitis be prevented?
While not all cases of pancreatitis can be prevented, there are steps you can take to reduce your risk. These include avoiding alcohol, quitting smoking, eating a healthy diet, and managing any underlying health conditions like gallstones or high triglyceride levels.
2. How long does it take to recover from pancreatitis?
Recovery time for pancreatitis varies depending on the severity of the condition and the underlying cause. Mild cases of acute pancreatitis may resolve within a few days with proper treatment, while severe cases may require weeks or even months of recovery. Chronic pancreatitis is a long-term condition that may require ongoing management.
3. Is pancreatitis hereditary?
In some cases, pancreatitis can run in families. Hereditary pancreatitis is a rare genetic condition that increases the risk of developing pancreatitis. However, most cases of pancreatitis are not hereditary and are instead caused by factors like alcohol use, gallstones, or certain medications.