Leukocytes, also known as white blood cells (WBCs), play an important role in your immune system. However, high levels of leukocytes in the urine can indicate an underlying problem with your urinary system. This article will discuss leukocytes in urine causes, symptoms, and treatment.
What are Leukocytes?
Leukocytes are a type of white blood cell that is part of your immune system. They help defend the body against infection and other foreign invaders. There are several different types of leukocytes, each with their own functions:
- Neutrophils: These are the most common leukocyte and are one of the first cell types to arrive at the site of infection. Neutrophils help destroy bacteria and other pathogens.
- Eosinophils: Responsible for combating multicellular parasites and infections. They also play a role in allergic reactions.
- Basophils: Release histamines and other chemicals that are involved in inflammatory responses.
- Lymphocytes: Includes both T cells and B cells that target specific pathogens and help activate the adaptive immune system.
- Monocytes: These largest types of white blood cells ingest and destroy pathogens and dead cells. They differentiate into macrophages that act as scavengers.
Normally, just a small number of leukocytes are present in urine. An excess amount indicates inflammation or infection somewhere in the urinary tract. When damage or microbial invasion occurs, leukocytes will be released from the bloodstream and travel to the site to fight infection.
Leukocytes produce chemicals to destroy invading pathogens. They also call in additional defender cells and stimulate other immune responses. These actions help fight and limit the infection.

What Causes Leukocytes in Urine?
There are several possible causes for leukocytes showing up in the urine:
1. Urinary Tract Infections
One of the most common reasons for high leukocyte levels is a urinary tract infection (UTI). UTIs occur when bacteria enter the urinary tract and multiply, most often in the bladder or urethra. Typical UTI symptoms include:
- Burning sensation when urinating
- Frequent urge to urinate
- Cloudy, bloody, or foul-smelling urine
- Pelvic pain or pressure
- Low grade fever in some cases
If left untreated, the infection can spread up to the kidneys and become even more serious. Once it reaches the kidneys, it is called pyelonephritis. Kidney infections come with additional symptoms like high fevers, chills, nausea and vomiting.
UTIs are more common in women due to their shorter urethras. Risk factors include pregnancy, diabetes, urinary catheters, family history, and recent sexual activity. Those with weaker immune systems also have an increased UTI risk.
2. Kidney Infections
A kidney infection, also called pyelonephritis, can also lead to increased leukocytes. Bacteria enter the kidneys from the bloodstream or spread from another part of the urinary tract, like an untreated bladder infection. In addition to the usual UTI symptoms, kidney infections may cause:
- Fevers and chills
- Pain in the back, side, or groin
- Nausea and vomiting
- Confusion or mental changes (in severe cases)
Kidney infections require prompt medical treatment. Some people may need hospitalization for IV antibiotics and fluid administration.
3. Kidney Stones
Kidney stones are solid deposits of minerals and salts that form in the kidneys. They can cause blockages in the urinary tract that obstruct the normal flow of urine. This obstruction leads to a buildup of bacteria, inflammation, and higher leukocyte levels as the body reacts to the stone. Symptoms of kidney stones include:
- Severe pain in the back, side, lower abdomen, or groin
- Pain that comes and goes in waves, increasing and decreasing in intensity
- Pink, red, or brown urine from blood mixing
- Cloudy or foul-smelling urine
- Nausea and vomiting
- Frequent need to urinate
Small stones may pass naturally, while larger ones sometimes require surgical removal. Medications can help relax the ureter to allow a stone to pass.
4. Tumors
Both cancerous and non-cancerous growths in the kidneys, bladder, or reproductive organs can sometimes increase leukocytes. As tumors expand, they can block the normal flow of urine and cause accumulation of bacteria. The leukocytes are released as the body reacts to the resulting infection.
Symptoms depend on the tumor size and location but may include:
- Visible blood in the urine
- Unexplained weight loss
- Low back or abdominal pain
- Swelling in the legs or abdomen
Diagnostic tests like CT scans and cystoscopy can identify tumors. Cancerous ones require specialized treatment plans.
5. Interstitial Cystitis
Interstitial cystitis (IC) is a chronic inflammatory condition affecting the bladder walls. It leads to scarring and reduced bladder capacity. Symptoms include bladder pressure, pelvic pain, and frequent urination. While not an infection, IC can cause inflammation and leukocytes in urine.
6. Autoimmune Disorders
Autoimmune conditions like lupus, rheumatoid arthritis, and Sjogren’s syndrome can sometimes spread inflammation to the kidneys and urinary tract. This results in elevated leukocyte counts as the immune system attacks the body’s own tissues.
7. Medication Side Effects
Certain medications like antibiotics, chemotherapy drugs, and some older diuretics have leukocytes as a potential side effect. Always review your medications with your doctor and report any urinary symptoms.
8. Other Causes
Less common causes of leukocytes in urine include:
- Tuberculosis
- Radiation therapy
- Kidney damage from high blood pressure or diabetes
- Bladder cancer
- Sexually transmitted infections like chlamydia and gonorrhea
- Structural problems causing urine backflow
Symptoms of High Leukocytes
The symptoms associated with excess leukocytes depend on the underlying condition. With a simple bladder infection, you’ll likely experience the usual UTI signs like burning with urination, pelvic discomfort, and foul-smelling urine.
Kidney infections, stones, and blockages more commonly cause back pain, nausea, vomiting, and fever along with urinary symptoms. Advanced kidney infections may also lead to mental status changes like confusion.
Tumors can cause blood in the urine, swelling, or lower back pain. Interstitial cystitis mainly causes bladder pressure and pain. In some cases, there may be no symptoms at all. Leukocytes are sometimes found incidentally through tests done for other reasons.
The only way to determine the exact cause is through proper diagnosis from your doctor. Notify them of any urinary symptoms you experience.
Diagnosing High Leukocytes in Urine
If urinary symptoms are present, your doctor can check for increased leukocytes through a urine test called a urinalysis. This simple test is done in a lab and checks your urine for:
- White blood cells
- Red blood cells
- Bacteria
- Proteins
- Crystal deposits
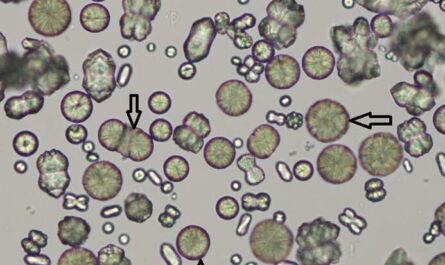
To evaluate the urine, both a dipstick test and microscopic examination are performed. The dipstick has special chemicals that change color in response to leukocytes and other substances. Under a microscope, technicians will count the number of white blood cells per high power field (WBC/HPF).
Normal urine should not contain more than 10 WBCs/HPF. Levels between 10-100 cells often indicate inflammation like a developing infection. Over 100 cells usually signals an active infection.